Before I leave the topic of our previous three blogs, I wanted to discuss a relatively new form of cardiomyopathy. Described first in Japan in 1991, Takotsubo cardiomyopathy or Takotsubo syndrome (hereafter abbreviated TTS) has been increasingly recognized as a fairly frequent type of cardiac dysfunction. Also called “broken heart syndrome” and “transient apical ballooning syndrome,” the name derives from the appearance of the left ventricle, which contracts normally at the base, but fails to contract or actually balloons outward at the apex, giving the appearance of a Japanese takotsubo (“octopus trap” in English).
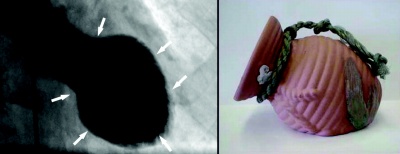
TTS is generally brought on by acute emotional or physical stress, as was the case in one of my patients recently. She is 74 years old and lost her son a year ago. On the anniversary of his death, she was thinking about him and woke up in the morning with sub-sternal chest pressure, as well as shortness of breath. When she went to the hospital, her EKG was abnormal and there was concern that she was having a heart attack. She was taken promptly to the cath lab, where angiography revealed her coronary arteries to be completely normal. Imaging of her left ventricle demonstrated a typical Takotsubo pattern (see images below, which is not my patient, but shows the typical findings).
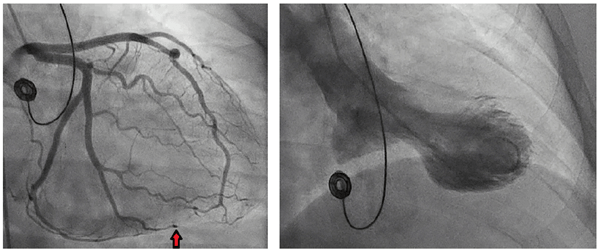
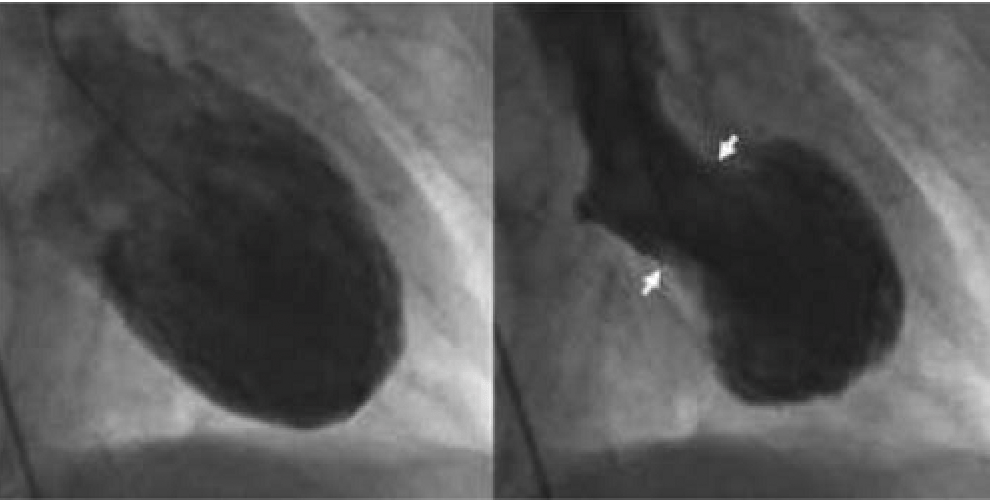
And in the next images, you can see the heart during diastole, when it is relaxed, and during systole, when it has contracted, demonstrating more clearly what parts of the heart are moving and what parts aren’t.
My patient was treated with a combination of aspirin and carvedilol, which is a beta blocker, a drug that blocks adrenaline and has been discussed in previous blogs. Her symptoms improved and she was able to go home the next day. On a follow-up echocardiogram three weeks later, her heart function had returned to normal.
My patient demonstrates several features that are typical of TTS. First is the precipitant of something stressful, in her case the emotional stress of thinking about her son, who had diedl. It should be noted that physical stressors—like a bad infection, an asthma attack or a stroke—can also cause TTS. The vast majority of patients with this condition can recall a stressful event leading up to the chest pain and shortness of breath, which are the usual symptoms of TTS (chest pain more consistently described than shortness of breath). Also, she is female and about 90% of patients with this condition are women.
She also demonstrated the rapid recovery seen with TTS. While some patients can present with cardiogenic shock due to the severe heart dysfunction, most are not that sick. And almost all patients show normalization or significant improvement in their heart function within weeks or a couple months.
No one knows the exact cause of TTS, but data support that an overabundant release of adrenaline—which can stun the heart—plays an important role. For this reason, beta blockers are a key component of acute and early post-TTS care. I keep many of my patients on a beta blocker long-term, particularly patients who have experienced this condition on more than one occasion. Those patients who present with cardiogenic shock and low blood pressure, though, cannot immediately be started on beta blockers and require medication to support the blood pressure.
TTS can be very scary to experience and lead some patients to become extremely ill. The good news is that most people survive and few people have any long-term consequences of the event. But it is a reminder once again—if you experience acute chest pain or shortness of breath, go to the hospital immediately. You might be having a “run of the mill” heart attack or you might have TTS, which requires in-hospital monitoring and treatment. In either case, time is essential. Don’t delay care and put your life at risk.
Greg Koshkarian, MD, FACC
