After an early summer hiatus from these weekly blogs, I’ll return this week to the question in the title above, which I get asked about almost daily in my office. The causes of swollen ankles are numerous, but most people’s biggest fear is that they have CHF (congestive heart failure). Indeed, peripheral edema (edema fluid causing swelling of the extremities, usually the legs) is often seen with CHF, and probably is its most visible manifestation. In that situation, it is caused by an increase in the pressures in the veins as the body tries to “help” the heart pump out more blood by retaining salt and water to expand fluid volume in the body.
We respond to a diminished output of blood from the heart by activating mechanisms to retain fluid (mostly via the kidneys) and shift blood from the periphery to the heart (by constricting the veins, where most of our blood volume is located). This leads to an increase in what we call “filling pressures,” the pressure in the heart during relaxation, creating a “slingshot effect,” where the heart is stretched a bit more right before it contracts, leading to an increase in the force of the contraction. This helps augment the output of blood to the body. But it comes at a cost—increased venous pressure in the body and in the lungs.
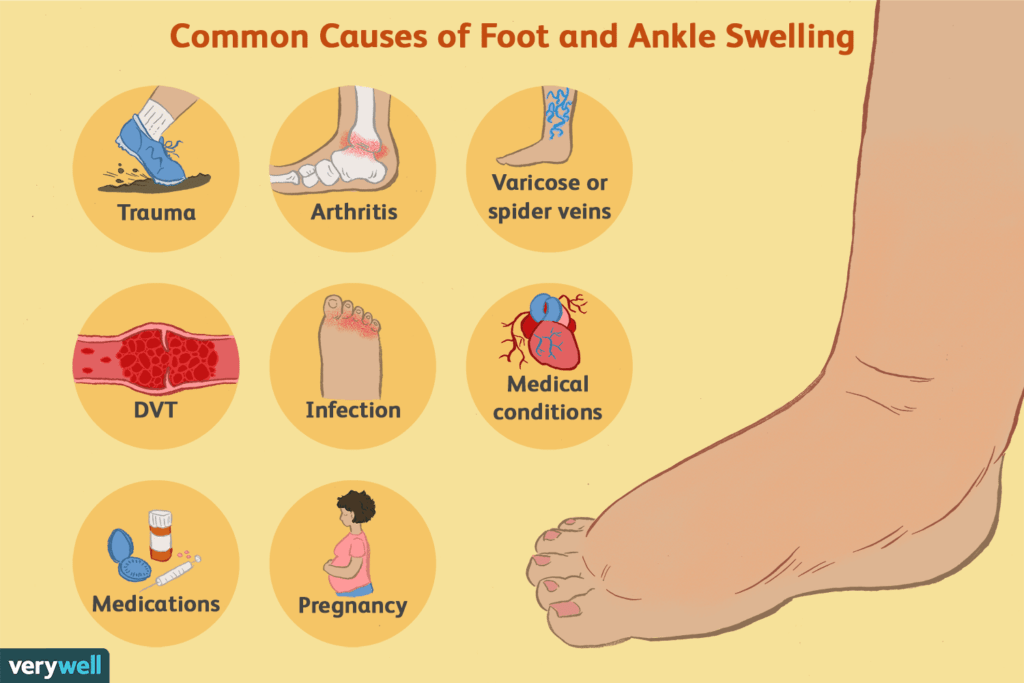
Increased pressures inside of veins tends to force fluid outward, as veins are not perfectly sealed tubes and have a certain degree of inherent “leakiness.” However, CHF is not the only condition that leads to increased pressure in the veins—and increased pressure is not the only mechanism that leads to fluid leaking out. Below is a schematic that lists many of the causes of swelling. I’ll highlight some of them.
Looking specifically at the veins themselves, DVT (deep vein thrombosis) means that a clot has obstructed the return of blood from the leg (or, more rarely, the arm). The obstruction leads to an increase in pressure in the vein behind the clot and thus edema with swelling. Venous insufficiency (including varicose veins) is when the venous system isn’t working properly, and pressure rises in the leg veins. Somewhat related is lymphedema, where there is obstruction of the lymphatic system. The lymphatics “soak up” excess fluid outside the veins and return it to the venous system. If the lymphatic system is obstructed, edema results.
Regarding medical conditions, we already talked about CHF. But kidney and liver problems can also cause edema. Kidney failure leads to fluid retention throughout the body, while liver failure leads to a loss of production of a protein called albumin, which acts like a “sponge” to hold fluid inside the vessel. When the liver doesn’t make enough albumin (or the kidneys don’t hold onto it and it exits the body in the urine—a condition called nephrotic syndrome), edema develops.
Then there are so-called hydrostatic (Latin for “water not moving”) causes of edema: sitting for long periods of time (at a desk job, on a long car or plane trip), or standing for too long (for instance, at a party, or in church, at a sporting event, at a political event).
Other causes include: medications—calcium channel blockers like amlodipine are notorious, as well as NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen or naproxen, which lead to fluid retention; pregnancy, due to the gravid uterus compressing the veins in the pelvis and impeding the outflow of blood from the legs; obesity, which also leads to vein and lymphatic compression; and hot weather (a big cause during summertime here in Tucson!), as one of the ways the body dissipates heat is to make the blood vessels more leaky.
So, what should you do if you notice swelling in your legs? If you sit or stand for long periods of time, walk around more frequently—or at least move your legs to activate the muscles, which helps blood circulate better. When sitting, prop your legs up on a stool or ottoman. Back off on NSAIDs if you are taking them. Look at your other medications to see if they are associated with swelling.
If simple maneuvers don’t work, see your doctor—particularly if there is tenderness or redness with the swelling, which could indicate a DVT. You may need to be checked for a heart or other organ (kidney or liver) problem. And there are also ways to diagnose and treat venous insufficiency. While edema doesn’t always mean CHF, it is still a finding that should elicit an evaluation.
Greg Koshkarian, MD, FACC
